
Dry Eye Disease – A Common Eye Problem Disturbing Daily Life
Dry eye disease is a common and often chronic problem, affecting daily life and activity of people of all ages. Dry eyes develop when the tears are not able to provide adequate lubrication for the eyes. This is typically caused by decreased tear production and increased tear evaporation. Besides interfering with quality of life, if this condition is left untreated, it might potentially lead to serious complications including eye infections, abrasion of the corneal surface, corneal ulcers and visual loss.
Get To Know Tear Film
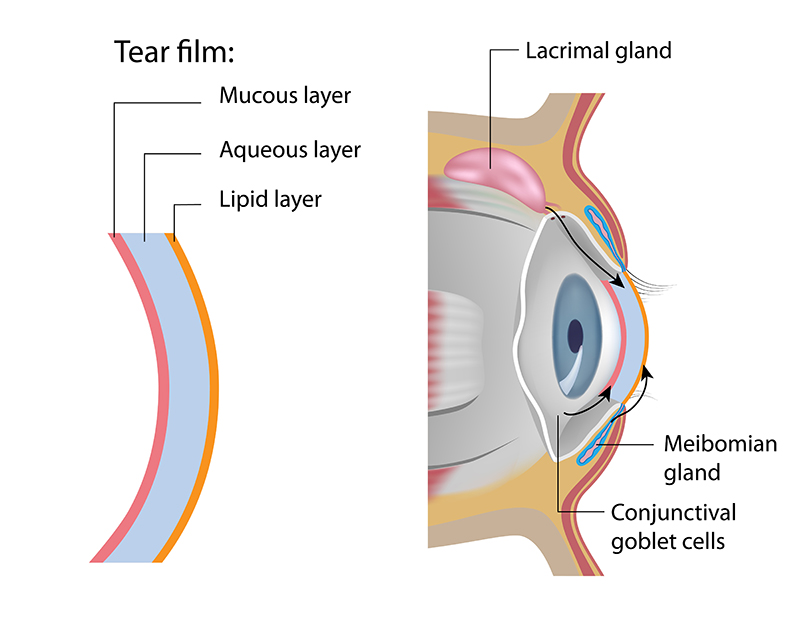
The tear film covers the normal ocular surface. It comprises the following 3 layers, extending from the outer to inner layers:
- Lipid layer: Lipid layer is produced by the Meibomian glands which are the tiny oil glands which line along the margin of the upper and lower eyelids. As the outermost layer of the tear film, lipid layer is an essential component of the tear film, providing a smooth optical surface and retarding evaporation from the eye.
- Aqueous layer: Aqueous layer is produced by the lacrimal glands. Aqueous layer is primarily composed of water which is the main component of tears.
- Mucin layer: The mucin layer – the innermost layer of the tear film is produced by the goblet cells located in conjunctiva. Mucin layer allows the watery layer to spread evenly over the surface of the eye, enabling the eye to remain moist and lubricated.
These three layers work collaboratively to help maintain the health of the eyes and prevent eye infection. Problems with any of these layers can cause dry eyes varied in types and characteristics.
Warning Signs And Symptoms Of Dry Eyes
- Eye irritation or eye discomfort
- A stinging, burning or scratchy sensation in the eyes
- Eye redness with stringy mucus around the eyes
- Sensitivity to light or watery eyes which is the body’s response to the irritation of dry eyes
- Blurred vision or eye fatigue
- A sensation of having foreign body in the eyes
- Difficulty opening eyes, especially in the morning
If any signs and symptoms of dry eyes exhibit, it is highly advised to seek medical attention and further investigation provided by the expert ophthalmologist, allowing for accurate diagnosis and effective treatment before complications arise.
Causes Of Dry Eyes
A variety of factors can disrupt the healthy tear film. Main causes of dry eyes are classified into:
- Aqueous tear deficiency: Dry eyes can develop when aqueous fluid cannot be sufficiently produced. This condition is commonly found in:
- Certain medical conditions including Sjogren’s syndrome and other autoimmune diseases, e.g. rheumatoid arthritis and systemic lupus erythematosus (SLE)
- Non Sjogren’s syndrome, such as congenital lacrimal duct obstruction, immunocompromized conditions, severe drug allergy, eye inflammation causing lacrimal duct obstruction, corneal inflammation (keratitis), and corneal nerve desensitivity caused by long-term contact lens use.
- Hormonal changes. In combination with aging, changes in the level of sex hormones, particularly in menopausal women greatly contribute to a significant reduction in aqueous fluid and mucus production.
- Certain medications, including antihistamines, nasal decongestants, antihypertensive agents and certain antidepressants.
- Increased tear evaporation (evaporative dry eyes): Common causes of increased tear evaporation are:
- Meibomian gland dysfunction or obstruction. Meibomian gland dysfunction is characterized by blockage, inflammation or other abnormalities of the meibomian glands that results in impaired lipid secretion, leading to evaporative dry eye.
- Eyelid abnormalities, such as the eyelids turning outward and inward, causing a gap while closing eyes and blinking less often which tends to occur when concentrating during certain activities, such as reading and driving.
- Severe eye damages after exposure to chemicals or severe drug allergy. As a result of severe corneal inflammation, corneal scar is formed, affecting the production of mucins in the layer which adheres firmly to the cornea and conjunctiva.
- Eyestrain from overuse of digital devices and contact lenses. Computer eye strain can cause meibomian gland dysfunction due to a reduction in blinking that leads to less lipid and aqueous secretion and eventually tear film instability and rapid evaporation.
 Treating The Underlying Cause Of Dry Eyes
Treating The Underlying Cause Of Dry Eyes
In most cases, treating an underlying health problem can help alleviate the symptoms of dry eyes. Nevertheless, there are numerous factors contributing to dry eyes, including:
- Certain medical conditions, medications and other factors affecting the production of aqueous tear, such as systemic lupus erythematosus (SLE) and rheumatoid arthritis. In such a case, these underlying conditions must be treated or well-controlled, allowing for an adequate tear production. For instance, if some medications are causing dry eyes, the doctor may consider replacing them with other medications, those do not induce dry eyes. Once the underlying causes are properly addressed and corrected, dry eyes often improve and gradually subside.
- Rapid tear evaporation caused by eyelid inflammation or abnormalities. If meibomian glands inflame or do not function properly, lipid secretion turns to be cloudy and sticky, leading to the obstruction of the gland openings on the edge of eyelids. To treat eyelid inflammations and meibomian gland obstruction, applying warm compression and eyelid cleansing are a mainstay of treatment. In case that eyelids turned outwards, eyelid surgery might be considered, if appropriate.
- Unhealthy lifestyle and environment. To minimize the recurrence of dry eyes, it is crucial to strictly refrain from certain factors those trigger the symptoms. These include avoiding air blowing in the eyes from hair dryer, fan or air-conditioner, taking eye breaks during long tasks, positioning computer screen below eye level and considering wearing wraparound sunglasses or other protective eyewear. If necessary, artificial tears can be used regularly to keep the eyes well lubricated.
Treatment And Lid Hygiene
Some medications aim to reverse or manage conditions that cause dry eyes while other treatments can enhance tear quality or prevent tears from quickly evaporating from the eyes. Medications used to treat dry eyes include:
- Artificial tears: Artificial tears help to control mild dry eye symptoms. Classified by the ingredients, there are two categories of artificial tears:
- Artificial tears with preservative: Preservatives are additive substances added to prevent contamination after opening the cap. Some preservatives are biodegradable and disappearing after exposure to the eye tissue or light. Artificial tears with preservative are usually recommended for patients with mild to moderate dry eyes. Since using the preservative drops can cause eye irritation, therefore they are limited to be used up to 4 times a day, in the morning, noon, evening and before bedtime. If dry eyes persist or progress, non-preservative drops might be prescribed as a more suitable option.
- Artificial tears without preservative: Non-preservative artificial tears are normally available in small single dose container/nebule which last 24 hours after opening. Some non-preservative artificial tears are present as bottles with specially designed one-way valve, allowing for a prolonged usage without contamination which can be used up to 6 months. Since non-preservative drops are considered safe, they can be used as often as needed, e.g. every 1-2 hours. Not only patients with severe dry eyes, but non-preservative drops are also recommended for patients with mild to moderate symptoms.
Although several dosage forms of artificial tears are available, they seem to pose different components and advantages. Eyedrops with various concentrations and viscosity are clear solution that can be used at any time including daytime as they do not interfere much with the vision. While lubricating eye ointments or gels coat the eyes and provide longer lasting effect. However, ointments and gels are much thicker than eyedrops which cloud the vision. Therefore, ointments and gels are best used before bedtime.
- Tear-stimulating drugs: Drugs recognized as tear secretogogues, e.g. diquafosol help increase tear production in both aqueous and mucin layers.
- Antibiotic drugs: Antibiotic drugs, such as doxycyline are used to reduce inflammation and modify tear components.
- Corticosteroids: Short term steroids eye drops are used to reduce corneal inflammation which happened in dry eyes. Corticosteroids, however, are not ideal for long-term use due to a number of side effects.
- Immune-suppressing medications: Immunosuppressants, such as cyclosporine eyedrops can suppress the inflammation on the surface of cornea, increasing tear production while mitigating symptoms of dry eyes. It is safer than corticosteroids for long-term use.
- Warm compression and lid hygiene: Lid hygiene is essential for good eye care to decrease obstruction of lipid glands and enhance lipid secretion from meibomian glands, enabling the tear film to lubricate the ocular surface more efficiently. Warm compression with eyelid cleansing and massage can be performed simply by using pads wetted in the eyelid cleansing solutions or diluted baby shampoo mixed with clean water for cleaning the edge of eyelids, allowing for unclogging the obstruction of meibomian glands.
- Autologous blood serum drops. Eye drops derived from a patient’s own blood may be an option if severe dry eye symptoms do not respond to other treatments. Autologous blood serum contains certain biological substances that accelerate the tissue recovery process from injuries. This new approach has gained therapeutic standing by reducing cell and tissue inflammations. To make these eyedrops, a sample of a patient’s blood is processed to remove the red blood cells in order to obtain serum which is then mixed with sterile balanced salt solution.
- Plugging tear drainage ducts. This procedure intends to keep and preserve the tears on ocular surface by plugging the openings to the tear drainage ducts (punctum) which connect to the nose either with tiny silicone plugs (punctal plugs) or punctal cautery, using heat to burn the tear drainage duct opening as permanent solution in very severe cases. Punctal cauterization is an effective modality in treating extremely severe dry eyes or patients who repeatedly lose their punctal plugs.
Vision Loss As Potentially Serious Complication Of Dry Eyes
Most cases with dry eyes only experience mild to moderate symptoms which respond considerably well to standard treatments. Nevertheless, some patients who have underlying health issues, e.g. rheumatoid arthritis and advanced SLE, severe drug allergic reactions, severe burns or chemical exposure are at greater risks of developing extremely severe or progressive dry eyes. Severe dry eyes can substantially lead to eye infection and inflammation, abrasion of the corneal surface, persistent non-healing wound on cornea, corneal ulcers, perforation and even visual loss. Thus, the attention must be immediately raised if any signs or symptoms of dry eyes indicate.
Prevention Of Dry Eyes
Lifestyle modification plays a crucial role in minimizing the risk of developing dry eyes. Changes can be as simple as remembering to:
- Take regular breaks from activities, e.g. watching TV, using a computer or digital devices and reading for long periods. During using computer screen or mobile phone, to enhance eye comfort, it is recommended to look away from the screen every 20 minutes and look at something around 20 feet away for about 20 seconds.
- Avoid wearing the contact lenses for a long period of time. Eyeglasses should be worn alternately.
- Have proper lighting while using computer and other digital gadgets
- Blink frequently to keep the eyes moist and lubricated.
- Wear protective sunglasses while staying in dry, warm or windy environment.
- Consume adequate five food groups while eating more foods high in omega 3 fatty acid which act as antioxidant that might aid in reducing eye inflammation and alleviating symptoms of dry eyes.
Dry eyes are common and often a chronic problem, affecting daily life and quality of life. If prolonged signs and symptoms of dry eyes exhibit after lifestyle changes, medical assistance provided by the ophthalmologist must be sought in order to receive additional investigation, leading to effective treatment before other serious complications develop.


Leave a Reply
You must be logged in to post a comment.